Immunotherapy has revolutionized cancer treatment. However, immunologically cold tumors, including glioblastoma (GBM), the most common primary malignant brain tumor in adults, are not responsive well to current T cell-based immunotherapies such as checkpoint blockade. These challenges are largely due to the immunosuppressive microenvironment that impedes T cell function. A mission of our research is to develop effective therapeutic strategy to reprogram tumor immune microenvironment, which allows T or NK cells to attack the tumor cells. The key target we have chosen is tumor-associated macrophages (Mfs) that are immune-hostile and usually are the major non-neoplastic cells in the tumor mass.
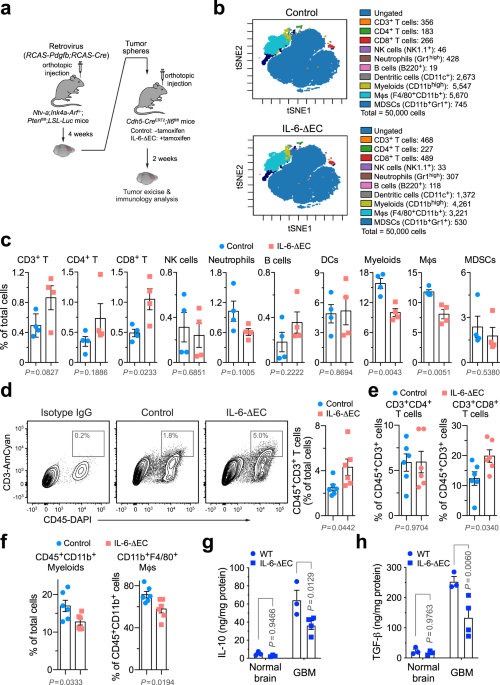
Our journey began several years ago with unusual observation: immunosuppressive Mfs stay proximately to blood vessels within the GBM tumors [1]. Our following study revealed a vascular niche effect, through which tumor endothelial cells (ECs) secrete IL-6 to drive Mfs toward alternative activation, a cellular status with immunosuppressive phenotypes. Inspired by these findings, we tested an IL-6-neutralizing antibody-based therapy in a genetically engineered mouse GBM model, which shows a modest therapeutic efficacy [1]. Interestingly, about a year later, another group from Northwestern University, led by Dr. Orin Bloch, published an elegant paper, verifying the therapeutic effects of anti-IL-6 treatment in syngeneic mouse GBM models including GL261 [2]. These encouraging results led us to further explore anti-IL-6 treatment as adjuvant immunotherapy with immune checkpoint blockade against GBM. However, our data show that IL-6 inhibition does not synergize PD-1 and CTLA-4 checkpoint blockade in our genetic model [3]. To understand the mechanism leading to this “failure” and to further develop additional approaches to strengthen the treatment, we performed RNAseq analysis in IL-6-treated Mfs. This unbiased transcriptome analysis validated the pro-tumor role for IL-6 in alternative Mϕ activation and production of immunosuppressive IL-10, consistent with our previous work [1]. Strikingly, we found out that IL-6 unexpectedly stimulates the expression of CD40, a co-stimulation molecule that is known to induce anti-tumor Mf activation. As such, we think that there is a dual role of IL-6 in regulating Mϕ activity, including pro-inflammatory (stimulation of CD40 expression) and anti-inflammatory (induction of alternative Mϕ activation and immunosuppression) functions. Likewise, monotherapy against IL-6 ends up with deactivating CD40 signal, which is an essential co-stimulatory signal for T cell activation, likely explaining the reason why anti-IL-6 alone failed to sensitize immune checkpoint blockade. Based on these findings, we designed a dual-targeting strategy, anti-IL-6 plus pro-CD40, to synergistically activate tumor-associated Mfs. It worked! The dual-targeting treatment reduces populations of immunosuppressive IL10+F4/80+ Mfs and increases cytotoxic CD8+ T cell infiltration and activation. Notably, the cocktail containing antibodies against IL-6, CD40, PD-1, and CTLA-4 exhibits robust therapeutic efficacy in two syngeneic GBM mouse models, almost doubling animal survival in the genetically engineered mouse GBM model and inducing complete tumor regression in the GL261 model [3].
In summary, this study leads us to develop a new therapeutic strategy, namely, antibody cocktail-based immunotherapy that combines checkpoint blockade with dual-targeting of IL-6 and CD40, this strategy would be feasible, convenient, and hopefully, effective. We hope to initialize clinical trials in the near future, with immune checkpoint inhibitors plus neutralizing antibodies against IL-6 or IL-6 receptor, such as tocilizumab or sarilumab, and anti-CD40 agonist antibodies, such as APX005M, in human patients with GBM or possibly with other immunologically cold tumors, such as pancreatic, ovarian, and prostate cancers.
We encourage readers to find more details in our full-text publication.

A schematic model. (Figure created with BioRender.com)

- Wang Q, He Z, Huang M, Liu T, Xu H, Ma P, Zhang L, Zamvil SS, Hidalgo J, Zhang Z, O’Rourke DM, Dahmane N, Brem S, Gong Y, & Fan Y. Vascular niche IL-6 induces alternative macrophage polarization in glioblastoma through HIF-2a. Nature Comm. 2018; 9:559.
- Lamano JB, Lamano JB, Li YD, DiDomenico JD, Choy W, Veliceasa D, Oyon DE, Fakurnejad S, Ampie L, Kesavabhotla K, Kaur R , Kaur G, Biyashev D, Unruh DJ , Horbinski CM, James CD, Parsa AT, & Bloch O. Glioblastoma-Derived IL6 Induces Immunosuppressive Peripheral Myeloid Cell PD-L1 and Promotes Tumor Growth. Clin Cancer Res. 2019;25(12):3643-57.
- Yang F, He Z, Duan H, Zhang D, Li J, Yang H, Dorsey JF, Zou W, Nabavizadeh SA, Bagley SJ, Abdullah K, Brem S, Zhang L, Xu X, Byrne KT, Vonderheide RH, Gong Y, & Fan Y. Synergistic immunotherapy of glioblastoma by dual targeting of IL-6 and CD40. Nat Commun 12, 3424 (2021). https://doi.org/10.1038/s41467-021-23832-3





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in