Connect the dots: HCC and NK cell
Back when I was a medical student in China, I saw a lot of hepatocellular carcinoma (HCC) patients who were suffering badly from this terrible disease. At the end of the battle, not only were these families broke, but they had also lost their loved ones.
As a young medical student, I didn’t have much understanding of this disease. For example, how does the hepatitis B virus (HBV) cause the HCC? What I learned in my immunology and medicine classroom is: although there are many factors attributing to the disease's progress, immune response is one of the key factors for HCC development. To gain more insight about the virus, immune response, and cancer development, after finishing my medical training, I decided to pursue a Ph.D. training in immunology, one of the most complex, fast-growing subjects in science. However, during my Ph.D. training, I mainly focused on NK cell immunobiology. There wasn’t much research directly related to the virus, immune response, and HCC.
After my Ph.D. training, I realized that the best environment at the time to continue NK work was in the USA, I applied and was accepted to an NIH fellowship training position. My research projects heavily concentrated on NK cell biology again, with a focus on cytotoxic and inhibitory immunological synapses (an interface between immune cells and target cells) 1,2. I was doing very well in NIH, but I was still wondering about how these basic immunobiology findings could be converted into a meaningful value for patients.
At the end of my postdoctoral fellowship at NIH, I was still eager to do translational medicine-related research. So, I competed for a Ragon Fellowship award (Ragon Institute of MGH, MIT, and Harvard) to extend my microscopy-based studies of immunological synapses of NK cells to those formed by HIV-specific cytotoxic T lymphocyte (CTL) cells from elite controllers and chronic progressors. This is the first time that I got in touch with virus-related, patient-orientated immunological research. I was so excited about this opportunity.
After joining Baylor College of Medicine (BCM) in 2012 to run my own independent research lab, I continued to investigate NK cell biology. But, this time, I really wanted to combine NK cells and virally infected diseases. This motivation originated from my early medical training when I was still a medical student, as well as the HIV training from when I was in Ragon Institute.
I really wanted to help these HCC patients and their families because I still recalled their battles with the HBV infection and HCC from when I was a medical student. HBV infection became the main cause of HCC in China. More than 53% of worldwide HCC patients comes from China, which accounts for the second most common cancer in China. HCC is relatively rare (~ six new cases of HCC per every 100,000 people) in the USA, but the number of HCC patients in the USA has risen.
The biggest problem for HCC treatment is that more than 100,000 patients each year ( https://gco.iarc.fr/today/home) with relapsed or refractory HCC have not responded to standard treatment 3. In addition to viral cytopathic effects (CPEs), host immune responses, such as CTL and NK cells, also contribute to liver damage and HCC development.
As an immunologist, I am wondering whether I can do something for the HCC patients. NK cells are highly enriched in the human liver (Figure 1). The percentage of NK cells in the total intrahepatic lymphocytes in human and mouse livers are 25-40% and 10-20%, respectively 4.
 |
|
Figure 1: Comparison of cell composition of blood (A) and healthy liver (B). (A) Blood components are listed in the first layer, including plasma (55% by volume), red blood cells (45% by volume), platelets, and leukocytes (< 1%). Leukocytes (another name for white blood cells) can be further classified as non-lymphocytes (60-80% by number, e.g., neutrophils, monocytes, eosinophils, etc.) and lymphocytes (20-40% by number, e.g., T, NK, and B cells). NK cells account for around 10-20% of the total lymphocytes by which is divided into two main subsets: 90% of mature CD56dim and 10% of less mature CD56bright 5. The CD56dim subset in the peripheral blood has high granule contents and is composed of canonical and adaptive populations 6. (B) Liver is the frontline immune organ. Hepatocytes constitute about two thirds of total cell population in the liver 7. The average human liver contains about 1010 lymphocytes. About 50% of hepatic lymphocytes are NK cells (30-50%) 8. These liver NK cells are equally divided into CD56dim and CD56bright. The CD56bright liver NK cells can be classified as liver-resident (lr-NK), memory-like (ml-NK), and transient conventional (cNK) NK cells 9. Approximately 50% of the hepatic CD56bright NK cells is lr-NK that is further subdivided into CD49a+, CD49e-, and Eomeshi subsets, each subset with a distinct function 10-12. ND, no data. Modified from Racanelli et al 7 and with the help from Minh Ma. |
The percentage of intrahepatic NK cells in the liver is around 5 times higher than the percentage of peripheral blood NK cells in humans 13,14. The liver is the largest solid organ of the human body, which is responsible for the removal of pathogens such as bacteria from systemic circulation 15. NK cells can quickly provide the first line of defense in the liver tissue, which explains the highly enriched NK lymphocyte populations in the liver.
In 2012, the use of chimeric antigen receptors (CARs) to redirect CTLs towards cancer or infected cells 16-18 has become a promising approach to overcome antigen restriction or escape mutations 19-21. Given the NK training and medical background, I was curious to know whether we could use CAR-NK for HCC treatment. So, I started to connect the dots between HCC and NK cells when I looked back.
The first thing we need to identify is a targetable antigen on the HCC tumor cell surface. After the literature search and bioinformatic verification, our group selected the surface CD147 molecule as our target for HCC.
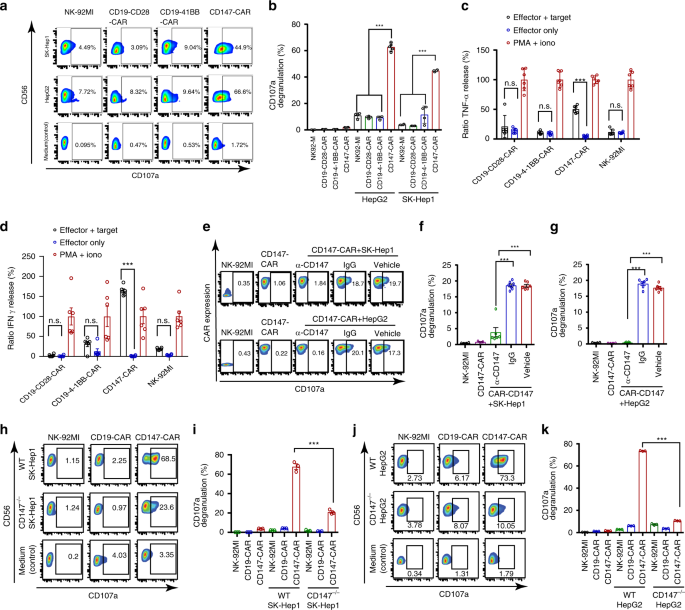
Next, to exploit the unique biology of CAR-NK cells (e.g., an ‘off-the-shelf’ universal CAR product, liver-enriched lymphocytes, and limited toxicity), we generated CAR-NK cells with a single-chain variable fragment (scFv) of CD147 to endow the specificity of NK cells, as well as intracellular domains to enhance persistence of NK cells.
To demonstrate the efficacy of CD147-CAR, we used the NK cell line (NK-92) first, then extended to primary NK and T cells in series of in vitro and in vivo assays using multiple systems.
After the demonstration of CD147-CAR’s effectiveness, we need to test the safety/toxicity of CD147-CAR. It is well-recognized that CAR-NK therapy has less severe toxicity in patients, compared to CAR-T therapy, but it is still crucial to test it in a number of pre-clinical studies. In order to further alleviate the “on-target, off-tumor” toxicity concern, we provide the data regarding GPC3-CAR in combination with CD147-SynNotch modified CAR cells. We also provided data for the strategy involving CD147-CAR in combination with GPC-3-SynNotch modified CAR cells, which provide a novel and safe ‘logic-gated’ cytotoxicity strategy for HCC treatment.
To further demonstrate safety, we generated a transgenic mouse model with the expression of a human CD147 transgene (hCD147TG). No severe toxicity has been observed in these hCD147TG mice when HCC-bearing hCD147TG mice were treated with CD147-CAR cells.
This work calls for the development of a clinical trial for HCC using CD147-CAR in the future.
https://www.nature.com/articles/s41467-020-18444-2
References
- Liu, D., et al. Integrin-dependent organization and bidirectional vesicular traffic at cytotoxic immune synapses. Immunity 31, 99-109 (2009).
- Liu, D., Peterson, M.E. & Long, E.O. The adaptor protein Crk controls activation and inhibition of natural killer cells. Immunity 36, 600-611 (2012).
- Yang, J.D., et al. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol 16, 589-604 (2019).
- Tian, Z., Chen, Y. & Gao, B. Natural killer cells in liver disease. Hepatology 57, 1654-1662 (2013).
- Michel, T., et al. Human CD56bright NK Cells: An Update. J Immunol 196, 2923-2931 (2016).
- Poli, A., Michel, T., Patil, N. & Zimmer, J. Revisiting the Functional Impact of NK Cells. Trends Immunol 39, 460-472 (2018).
- Racanelli, V. & Rehermann, B. The liver as an immunological organ. Hepatology 43, S54-62 (2006).
- Gao, B., Jeong, W.I. & Tian, Z. Liver: An organ with predominant innate immunity. Hepatology 47, 729-736 (2008).
- Mikulak, J., Bruni, E., Oriolo, F., Di Vito, C. & Mavilio, D. Hepatic Natural Killer Cells: Organ-Specific Sentinels of Liver Immune Homeostasis and Physiopathology. Front Immunol 10, 946 (2019).
- Male, V. Liver-Resident NK Cells: The Human Factor. Trends Immunol 38, 307-309 (2017).
- Wang, Y. & Zhang, C. The Roles of Liver-Resident Lymphocytes in Liver Diseases. Front Immunol 10, 1582 (2019).
- Hudspeth, K., et al. Human liver-resident CD56(bright)/CD16(neg) NK cells are retained within hepatic sinusoids via the engagement of CCR5 and CXCR6 pathways. J Autoimmun 66, 40-50 (2016).
- Liu, P., Chen, L. & Zhang, H. Natural Killer Cells in Liver Disease and Hepatocellular Carcinoma and the NK Cell-Based Immunotherapy. J Immunol Res 2018, 1206737 (2018).
- Sun, H., Sun, C., Tian, Z. & Xiao, W. NK cells in immunotolerant organs. Cell Mol Immunol 10, 202-212 (2013).
- Bogdanos, D.P., Gao, B. & Gershwin, M.E. Liver immunology. Compr Physiol 3, 567-598 (2013).
- Maldini, C.R., Ellis, G.I. & Riley, J.L. CAR T cells for infection, autoimmunity and allotransplantation. Nat Rev Immunol 18, 605-616 (2018).
- Kim, G.B., Hege, K. & Riley, J.L. CAR Talk: How Cancer-Specific CAR T Cells Can Instruct How to Build CAR T Cells to Cure HIV. Front Immunol 10, 2310 (2019).
- Leibman, R.S., et al. Supraphysiologic control over HIV-1 replication mediated by CD8 T cells expressing a re-engineered CD4-based chimeric antigen receptor. PLoS Pathog 13, e1006613 (2017).
- Gill, S. & June, C.H. Going viral: chimeric antigen receptor T-cell therapy for hematological malignancies. Immunological reviews 263, 68-89 (2015).
- Zhen, A., et al. HIV-specific Immunity Derived From Chimeric Antigen Receptor-engineered Stem Cells. Molecular therapy : the journal of the American Society of Gene Therapy 23, 1358-1367 (2015).
- Leibman, R.S. & Riley, J.L. Engineering T Cells to Functionally Cure HIV-1 Infection. Molecular therapy : the journal of the American Society of Gene Therapy 23, 1149-1159 (2015).




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in