Background
Metastatic breast cancer remains largely incurable and is estimated to be responsible for ~90% of cancer-related mortality. Metastases arise when tumor cells migrate out of the primary tumor and enter the bloodstream (in a process called “intravasation”) which carries them to distant organs. Once tumor cells exit the vasculature in these organs (a process called “extravasation”), they are able to grow into metastatic lesions. However, in some patients, tumor cells do not grow immediately, but instead remain in a “sleeping” or dormant state, sometimes for decades, before resuming proliferation to form overt metastases. While numerous breast cancer treatments are available, none are capable of preventing metastasis. Therefore, a better understanding of the mechanisms underlying the dissemination and dormancy of tumor cells is needed.
A growing body of literature shows that the microenvironment of the primary tumor primes disseminated tumor cells (DTCs) for dormant or proliferative fates at distant organs, and by doing so, influences metastatic outcomes (1). However, just how the primary tumor regulates the fate of DTCs remains poorly understood.
To understand how signals in the primary tumor microenvironment influence disseminating cells and their behavior in the secondary site, we developed an implantable Window for High-Resolution Intravital Imaging of the Lung (WHRIL) (2,3). The WHRIL allows a longitudinal view of the living lung, at sub-cellular resolution, over days to weeks, making it possible, for the first time, to follow the fate of individual DTCs throughout the process of lung metastasis.
Using this tool, we have been able to longitudinally track the fate of tumor cells that spontaneously disseminate from an orthotopic breast tumor as they arrive to the lung, and compare the fate of these cells with tumor cells that have been intravenously injected into the vasculature of mice, and thus are not exposed to the primary tumor signals. This allowed us to study the primary tumor’s influence on the initial steps of the metastatic cascade in the secondary site.
We found that, as was observed in Fidler’s seminal experiments in the 1970’s (4), tumor cells injected directly into the vasculature are rapidly cleared from the lung in just a few days. However, we were completely surprised by what we observed with spontaneously disseminated tumor cells. We found that a ten-fold higher percentage of spontaneously disseminating are retained in the lung and for a significantly longer period of time. This difference was confirmed across several animal models. We wondered what could be responsible for this difference.
Why are spontaneously disseminated tumor cells retained in the lung significantly longer and at higher numbers compared to intravenously injected tumor cells?
In order to address this question, we postulated that, if tumor cells are able to extravasate quickly, they would be subjected less to harsh mechanical trauma within the circulatory system. Therefore, we postulated that the increased rate of retention of spontaneously DTCs is due to a better ability to extravasate. To test this, we used the WHRIL to study the kinetics of extravasation for each individual DTC and found that spontaneously DTCs extravasated very rapidly in the lung parenchyma compared to intravenously injected tumor cells.
Why do spontaneously disseminated tumor cells extravasate more quickly compared to intravenously injected tumor cells?
Our previous studies demonstrated that, within the primary tumor, contact between macrophages and cancer cells leads to an increased expression of an isoform of the actin regulatory protein, Mena, called MenaINV (Mena Invasive), which in turn enhances tumor cell migration and intravasation (5,6). We hypothesized that MenaINV expression could play a similar role during extravasation at the secondary site, conferring to tumor cells the ability to cross the endothelium quickly. To test this, we performed gain- and loss-of-function experiments for MenaINV and studied the kinetics of extravasation using the WHRIL. Interestingly, we found that the overexpression of MenaINV significantly increased the ability of tumor cells to extravasate quickly in the lung parenchyma, while the inhibition of MenaINV drastically impaired the ability of tumor cells to extravasate. Therefore, our data demonstrate that spontaneously DTCs have an increased ability to extravasate quickly (compared to intravenously injected tumor cells) that is conferred by the expression of MenaINV.
Following the fate of each DTC after extravasation in both spontaneous and experimental models, we found that a majority of injected tumor cells died shortly after extravasation, while the majority of spontaneously DTCs survived as single and solitary tumor cells (without dying or proliferating), suggesting that they may have become dormant.
Are spontaneously disseminated tumor cells dormant after extravasation in the lung?
To investigate if spontaneously DTCs are dormant, we stained lung tissue sections from both the spontaneous and experimental models, and primary tumor tissues and circulating tumor cells from the spontaneous model, for one of the best markers of dormancy, NR2F1. We found that spontaneously DTCs become progressively more enriched in NR2F1 expression as they disseminate from the primary tumor to the lung and that this increase in expression is apparently not induced within the circulation. Together, this indicates that the induction happens within the primary tumor itself.
How spontaneously disseminated tumor cells acquire the expression of the dormancy marker NR2F1?
Given this progressive and dramatic increase in NR2F1 expression, we hypothesized that the dormancy program may be activated near to, or at, sites where tumor cells intravasate; locations along the vasculature called Tumor MicroEnvironment of Metastasis (TMEM) doorways (7,8). TMEM doorways are stable triple cell complexes composed of a MenaHigh tumor cell, a Tie2High macrophage, and a blood vessel endothelial cell, all in direct physical contact. Thus, programming for dormancy might be induced as migratory tumor cells approach and interact with TMEM doorways. To test this, we stained serial sections of primary breast tumor tissues for TMEM doorways and for NR2F1 and its target gene SOX9, which is also a pluripotency gene (9,10). Then we measured the relative distance from each NR2F1- and/or SOX9-positive tumor cell to its nearest TMEM doorway. We found that NR2F1- and/or SOX9-positive tumor cells were specifically enriched and associated with TMEM doorways.
How is the expression of the dormancy marker NR2F1 increased in tumor cells around TMEM doorways?
We postulated that macrophages (which are enriched around TMEM doorways) might induce the expression of NR2F1 in tumor cells. To test this, we systematically depleted macrophages in tumor-bearing mice with clodronate liposomes and quantified the percentage of NR2F1-positive tumor cells in primary tumors, circulating tumor cells, and lung tissues. We found a significant reduction of NR2F1-positive tumor cells in all sites (compared to control animals), indicating that tumor associated macrophages in the primary tumor play an important role in inducing the expression of NR2F1 in primary cancer cells that are destined to disseminate. We confirmed this role via tumor cell-macrophage co-cultures which led to tumor cell-NR2F1 induction.
Why our findings are important
Our study provides important insight into the contribution of primary tumor microenvironmental niches to cancer metastasis by identifying the manner in which these niches spawn subpopulations of DTCs that are primed for dormancy in the secondary site (Figure 1). These studies identify also a new set of markers that, if detected in the primary tumor, may determine which patients are more prone to carry dormant and therapy refractory systemic disease (Figure 1). The tools and models developed here may provide ways to identify novel targets on disseminated tumor cells that could prevent successful colonization of or increase clearance from the secondary site. Such an approach has been recently proven by our team through the targeting of NR2F1 (11).

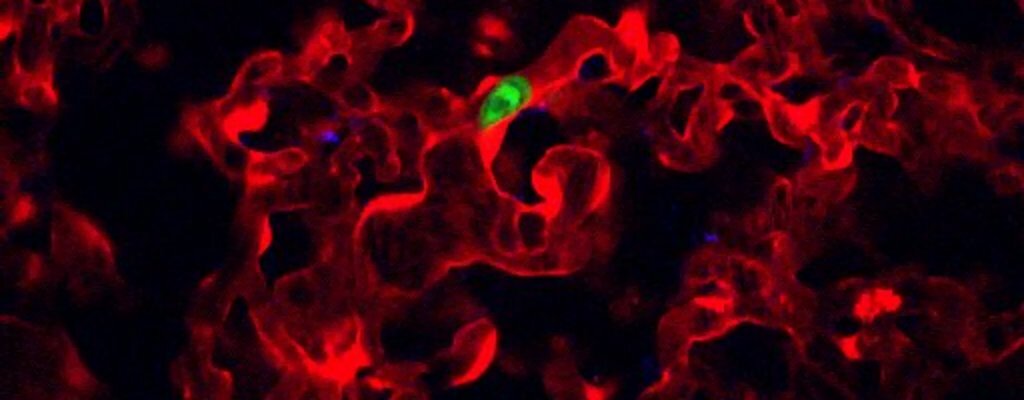
Figure 1. Model illustrating how the presence of a primary tumor programs disseminated tumor cells for stemness and dormancy at the secondary site. Left Panel: Within the primary tumor, migrating tumor cells are attracted to blood vessels. As they approach TMEM doorways (red triangle) on the vasculature, these tumor cells interact with macrophages and programs of dormancy (NR2F1) and invasion (MenaINV) are activated. Dormant cells also adopt cancer stem cell properties (SOX9). These cells then intravasate through TMEM doorways into the vasculature and become circulating tumor cells (CTCs). Right Panel: CTCs retain these programs at the secondary site where the invasion program (MenaINV) facilitates extravasation. The dormancy program expressed by these disseminated tumor cells (DTCs) keeps them as single cells.
References
- Fluegen G, Avivar-Valderas A, Wang Y, Padgen MR, Williams JK, Nobre AR, et al. Phenotypic heterogeneity of disseminated tumour cells is preset by primary tumour hypoxic microenvironments. Nat Cell Biol 2017;19:120-32
- Borriello L, Traub B, Coste A, Oktay MH, Entenberg D. A Permanent Window for Investigating Cancer Metastasis to the Lung. J Vis Exp 2021
- Entenberg D, Voiculescu S, Guo P, Borriello L, Wang Y, Karagiannis GS, et al. A permanent window for the murine lung enables high-resolution imaging of cancer metastasis. Nat Methods 2018;15:73-80
- Fidler IJ. Metastasis: quantitative analysis of distribution and fate of tumor emboli labeled with 125 I-5-iodo-2'-deoxyuridine. J Natl Cancer Inst 1970;45:773-82
- Pignatelli J, Bravo-Cordero JJ, Roh-Johnson M, Gandhi SJ, Wang Y, Chen X, et al. Macrophage-dependent tumor cell transendothelial migration is mediated by Notch1/MenaINV-initiated invadopodium formation. Sci Rep 2016;6:37874
- Roussos ET, Balsamo M, Alford SK, Wyckoff JB, Gligorijevic B, Wang Y, et al. Mena invasive (MenaINV) promotes multicellular streaming motility and transendothelial migration in a mouse model of breast cancer. J Cell Sci 2011;124:2120-31
- Harney AS, Arwert EN, Entenberg D, Wang Y, Guo P, Qian BZ, et al. Real-Time Imaging Reveals Local, Transient Vascular Permeability, and Tumor Cell Intravasation Stimulated by TIE2hi Macrophage-Derived VEGFA. Cancer Discovery 2015;5:932-43
- Oktay MH, Jones JG. TMEM: a novel breast cancer dissemination marker for the assessment of metastatic risk. Biomark Med 2015;9:81-4
- Hadjimichael C, Chanoumidou K, Papadopoulou N, Arampatzi P, Papamatheakis J, Kretsovali A. Common stemness regulators of embryonic and cancer stem cells. World J Stem Cells 2015;7:1150-84
- Sosa MS, Parikh F, Maia AG, Estrada Y, Bosch A, Bragado P, et al. NR2F1 controls tumour cell dormancy via SOX9- and RARbeta-driven quiescence programmes. Nat Commun 2015;6:6170
- Khalil BD, Sanchez R, Rahman T, Rodriguez-Tirado C, Moritsch S, Martinez AR, et al. An NR2F1-specific agonist suppresses metastasis by inducing cancer cell dormancy. J Exp Med 2022;219






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in